- Posterior segment complications from bone marrow transplants were seen in 13% of patients. Among the complications seen were vitreous hemorrhage, infectious retinitis, cotton-wool spots, and retinal detachment.
- Radiation retinopathy has been reported to occur in patients undergoing bone marrow transplant and high-dose chemotherapy and who received low-dose teletherapy. High-dose chemotherapy may lower the threshold for radiation retinopathy.
- Ocular ischemia evidenced by optic disc and retinal neovascularization may lead to tractional retinal detachment following chemotherapy and radiation therapy.
- Dry eye, keratitis, and cataracts may be sequelae of external beam radiation therapy with 3000-4000 rads. However, as little as 1150 rads may cause lenticular opacities.
- In one study, 82 ALL survivors and 15 AML survivors were followed for an average of 3 years. All of the AML survivors had a normal ocular examination. Cataracts developed in 52% of ALL survivors. However, only 1 patient suffered significant visual dysfunction as a result of ALL or its treatment.
Leukemias are a group of heterogeneous neoplastic disorders of white blood cells. Based on their origin, myeloid or lymphoid, they can be divided into two types. Leukemias traditionally have been designated as acute or chronic, based on their untreated course. Acute leukemias usually present as hemorrhage, anemia, infection, or infiltration of organs.
Many patients with chronic leukemias are asymptomatic. Other patients present with splenomegaly, fever, weight loss, malaise, frequent infections, bleeding, thrombosis, or lymphadenopathy. The image below depicts an impending retinal vein obstruction and intraretinal hemorrhage in a patient with chronic myelogenous leukemia. Some chronic leukemias enter a blast phase where the clinical manifestations are similar to the acute leukemias.
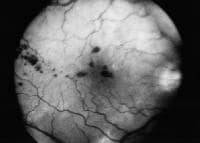 An impending bilateral central retinal vein obstruction was discovered during a routine examination of a 76-year-old man. Further workup revealed a WBC count of 709,000, a hemoglobin count of 12 mg/dL, and a platelet count of 104,000. The man was eventually diagnosed with CML. This image is a red-free photograph of the right fundus. Notice the intraretinal hemorrhages.
An impending bilateral central retinal vein obstruction was discovered during a routine examination of a 76-year-old man. Further workup revealed a WBC count of 709,000, a hemoglobin count of 12 mg/dL, and a platelet count of 104,000. The man was eventually diagnosed with CML. This image is a red-free photograph of the right fundus. Notice the intraretinal hemorrhages.
See Chronic Leukemias: 4 Cancers to Differentiate, a Critical Images slideshow, to help detect chronic leukemias and determine the specific type present.
Chronic myelogenous leukemia (CML) is characterized by an uncontrolled proliferation of granulocytes. An accompanying proliferation of erythroid cells and megakaryocytes is usually present. Many patients are asymptomatic but may present with splenomegaly, weight loss, malaise, bleeding, or thrombosis.
Chronic lymphocytic leukemia (CLL) represents a monoclonal expansion of lymphocytes. In 95% of cases, CLL is a predominantly malignant clonal disorder of B lymphocytes. The remainder is secondary to a T-cell clone. The neoplastic cell is a hypoproliferative, immunologically incompetent small lymphocyte. There is primary involvement of the bone marrow and secondary release into the peripheral blood. The recirculating lymphocytes selectively infiltrate the lymph nodes, the spleen, and the liver. Most patients are asymptomatic at diagnosis. As the disease progresses, lymphadenopathy, splenomegaly, and hepatomegaly develop. A secondary immune deficiency with hypogammaglobulinemia exists. A study by Wang et al found that when they studied the landscape of somatic mutations in chronic lymphocytic leukemia, pre-mRNA splicing was an important cellular process.[1]
Acute lymphocytic leukemia (ALL) is a malignant clonal disorder of the bone marrow lymphopoietic precursor cells. In ALL, progressive medullary and extramedullary accumulations of lymphoblasts are present that lack the potential for differentiation and maturation. An inhibition of the normal development of hematopoietic cell elements occurs. The clinical presentation is dominated by progressive weakness and fatigue secondary to anemia, infection secondary to leukopenia, and bleeding secondary to thrombocytopenia. When 50% of the bone marrow is replaced, then peripheral blood cytopenias are observed.
Acute myelogenous leukemia (AML) is a group of neoplastic disorders of the hematopoietic precursor cells of the bone marrow. AML is subdivided by the French-American-British system into 6 categories depending on the morphology. AML is not a disorder of rapidly proliferating neoplastic cells. The time for one cell division is prolonged with respect to that of normal bone marrow blast cells. A failure of maturation of the neoplastic cell clone exists. The bone marrow is gradually replaced by blast cells. Therefore, the most important complications are progressive anemia, leukopenia, and thrombocytopenia.
The treatment of leukemia is in constant flux, evolving and changing rapidly over the past few years. Most treatment protocols use systemic chemotherapy with or without radiotherapy. The basic strategy is to eliminate all detectable disease by using cytotoxic agents. To attain this goal, 3 phases are typically used, as follows: remission induction phase, consolidation phase, and maintenance therapy phase.
Chemotherapeutic agents are chosen that interfere with cell division. Tumor cells usually divide more rapidly than host cells, making them more vulnerable to the effects of chemotherapy. Primary treatment will be under the direction of a medical oncologist, radiation oncologist, and primary care physician. Although a general treatment plan will be outlined, the ophthalmologist does not prescribe or manage such treatment.
- The initial treatment of ALL uses various combinations of vincristine, prednisone, and L-asparaginase until a complete remission is obtained.
- Maintenance therapy with mercaptopurine is continued for 2-3 years following remission.
- Use of intrathecal methotrexate with or without cranial irradiation to cover the CNS varies from facility to facility.
- Daunorubicin, cytarabine, and thioguanine currently are used to obtain induction and remission of AML.
- Maintenance therapy for 8 months may lengthen remission. Once relapse has occurred, AML generally is curable only by bone marrow transplantation.
- Presently, treatment of CLL is palliative.
- CML is characterized by a leukocytosis greater than 100,000 cells. Emergent treatment with leukopheresis sometimes is necessary when leukostastic complications are present. Otherwise, busulfan or hydroxyurea may control WBC counts. During the chronic phase, treatment is palliative.
- When CML converts to the blastic phase, approximately one third of cases behave as ALL and respond to treatment with vincristine and prednisone. The remaining two thirds resemble AML but respond poorly to AML therapy.
- Allogeneic bone marrow transplant is the only curative therapy for CML. However, it carries a high early mortality rate.
- Leukemic retinopathy usually is not treated directly. As the hematological parameters normalize with systemic treatment, many of the ophthalmic signs resolve. There are reports that leukopheresis for hyperviscosity also may alleviate intraocular manifestations.
- When definite intraocular leukemic infiltrates fail to respond to systemic chemotherapy, direct radiation therapy is recommended.
- Relapse, manifested by anterior segment involvement, should be treated by radiation. In certain cases, subconjunctival chemotherapeutic agents have been injected.
- Optic nerve head infiltration in patients with ALL is an emergency and requires prompt radiation therapy to try to salvage some vision.
No comments:
Post a Comment